COPD stands for Chronic Obstructive Pulmonary Disease
According to the Global Burden Disease Study COPD stands for Chronic obstructive pulmonary disease was responsible for 251 million cases of COPD in 2016, out of those numbers it was estimated that 3.17 million people died as a result of the disease (5% of worldwide deaths that year) Considering that COPD could be avoided by lifestyle changes these figures make grim reading.
In this article, I would like to offer a little hope to people suffering from chronic obstructive pulmonary disease and its symptoms by telling you about a fantastic enzyme called Serrapeptase and its benefits to COPD.
One of the characteristics of COPD is mucus build-up, and the other one is inflammation, Serrapeptase has helped some people to minimize these symptoms of COPD and to have a better quality of life.
Please CLICK HERE to read their COPD success stories.
 What is COPD?
What is COPD?
If you have COPD then you will know that the disease is also known as chronic obstructive pulmonary disease, chronic bronchitis, or emphysema. You will also know that COPD gets worse over a period and it can be hard to breathe.
One of the symptoms of COPD is a bad cough that makes you bring up large amounts of dark-colored mucus other symptoms are wheezing, shortness of breath, and tightness around your chest as well as other symptoms.
Causes of COPD
If you were or are a smoker then you will know that smoking is the main cause of COPD, however, some people that have COPD never smoked a day in their lives (up to 25%) other factors may have contributed to their COPD such as:
- Pollution
- Dust
- Chemical fumes
A deficiency in alpha-1 antitrypsin may also lead to the development of COPD, however, it is rare.
Overview of COPD
To fully understand COPD, it is a good idea to understand how your lungs work. As you breathe in (inhale) the leading muscle of respiration (the diaphragm) tightens and moves down to make room in your chest, this motion creates space in your chest cavity and your lungs expand. The muscles between your ribs (intercoastal) may also expand and assist the chest cavity to enlarge, when you let the air out (exhale) the rib cage will pull itself upwards and outwards.
The air is sucked in through the nose and mouth as the lungs expand, and from there it travels into the windpipe and down into the lungs. The air then passes through the bronchial tubes and extends to the air sacs (alveoli)
The alveoli consist of a very thin wall surrounded by tiny blood vessels (capillaries) hemoglobin a red blood cell that assists in moving oxygen from the alveoli (air sacs) to the bloodstream. While this is happening carbon dioxide that has come from the heart past the pulmonary artery moves away from the capillaries and into the air sacs (alveoli) The pulmonary vein is responsible for delivering oxygen-rich blood to the left side of your heart, and from there the heart will pump the blood around the body.

Breathing Airways
What happens with your breathing?
We don’t usually think about our breathing unless we practice breathing exercises, breathing is quite a complicated process in the sense that other issues may affect the breathing process such as disease or injury. I’ll give you an example, your upper airways are lined with very fine hairs (cilia) their job is to catch all the germs that are in the air you are breathing in.
Germs from the air can lead to conditions like bronchitis (infection in the bronchial tubes) or if they go deep enough into your lungs they can develop into pneumonia. One of the main issues with the infection is the build-up of fluid or mucus, this will have an impact on the amount of air flowing into and out of your lungs.
Another example of how your breathing is affected is asthma, breathing in certain types of substances it will trigger an asthma attack which affects your breathing and makes it harder for the air to flow into and out of your lungs, I’m talking about irritants such as:
- Tobacco smoke
- Smoke from a wood-burning stove
- Strong perfumes
- Cleaning agents
- Dust
- Vapours
 Cigarette smoke
Cigarette smoke
Being exposed to cigarette smoke or other pollutants will cause damage to your airways and sacs, the damage will lead to COPD (chronic obstructive pulmonary disorder) as the condition prevents the proper flow of air into and out of the lungs, it can also curb the exchange of gas in the alveoli (air sacs)
Diaphragm
The smooth movement of your diaphragm as well as other muscles in your chest, neck & abdomen are key to your breathing. This smooth movement allows you to breathe in and breathe out, this movement is controlled by nerves in your brain, if damage were to occur to the nerves in the upper spinal cord it may stop your breathing altogether, in that case, a ventilator or respirator will be used to help you to breathe.
 Flow of blood
Flow of blood
The blood vessels that encompass the air sacs are pivotal for gas exchange, so a constant flow of blood is vitally important in this process. People who are inactive or have had surgery are susceptible to a blood clot or pulmonary embolism or PE. A pulmonary embolism can form a blockage to the lung artery reducing blood flow to the small blood vessels going to the lungs and inhibiting gas exchange.
The air that we breathe
When we breathe in the air it travels down through our windpipe and into the bronchial tubes or airways. The bronchial tube is made up of thousands of tiny, thin tubes called bronchioles, the bronchioles are the air sacs or alveoli. Small blood vessels or capillaries are located along the walls of the alveoli (air sacs) the air that passes through the air sacs and into the small capillaries contains oxygen. The gas exchange happens when carbon dioxide (CO2) a waste product is removed by oxygen. Your air sacs and airways are flexible meaning they can stretch, so when you take a breath one by one the air sacs fill with air much the same as a tiny balloon, when you exhale the air travels outwards.
COPD and airflow
If you have COPD the issue will be less airflow because:
- Mucus build-up will cause a blockage
- Damage to the air sacs
- Less elasticity in the air sacs
- Airways become inflamed and thicken
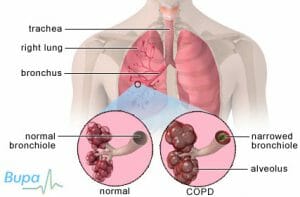 Picture of normal lungs and lungs that have COPD
Picture of normal lungs and lungs that have COPD
As you can see in normal the lungs are that of a normal healthy person, in COPD, you can see the damaged walls of the bronchioles and alveoli
Figure A shows the location of the lungs and airways in the body. The inset image shows a detailed cross-section of the bronchioles and alveoli. Figure B shows lungs damaged by COPD. The picture shows in detail a cross-section of the damaged bronchioles and alveoli walls.
In America, the condition COPD includes chronic bronchitis and emphysema, the difference being that in emphysema the walls of the air sacs are damaged whereas in chronic bronchitis the airways are nearly always inflamed or irritated. In emphysema, the walls of the air sacs change to a different shape affecting the amount of gas exchange in the lungs. In chronic bronchitis, the lining of the air sacs will swell because of the irritation and mucus build-up making it more difficult to breathe normally.
As with all versions of COPD, the symptoms and severity will vary from person to person
COPD Outlook
Chronic Obstructive Pulmonary Disorder can lead to a disability, after heart disease, cancer, and diabetes it is the next leading cause of death in the USA more than 16 million people have been diagnosed with COPD.
Because COPD starts and develops at a slow pace many people may not even be aware that they have it, often the symptoms will get worse over time and will have a detrimental effect on your daily life in the sense that you may not be able to do activities of daily living such as walking, housework, cooking, you may not even be able to mind yourself.
COPD isn’t a contagious disease, it is usually diagnosed in middle age or older age.
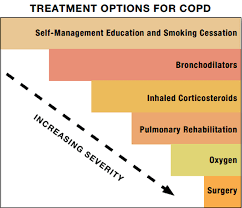
There is no cure for COPD yet, and doctors don’t have a solution to repair or reverse any damage that was done to the lungs, but there are some treatments and/or lifestyle changes that could help make feel better yourself, also to help you slow the progression of COPD.
How to live with Chronic obstructive pulmonary disease
It is important to look after yourself, these are things that you can do:
- Stop smoking
- Take your COPD meds (inhalers) to prevent a flare-up
- Get information from your doctor about nutritional supplements or painkillers.
- Exercise daily to improve your quality of life and symptoms
When it comes to exercise do as little or as much as you can do, don’t push yourself too much always get exercise advice before you start any new exercise program especially if you haven’t done any strenuous exercises for a while.
Weight
If you are overweight it is important to address this issue because the extra weight can contribute to breathlessness, which will put pressure on your heart and lungs, it can be done through a combination of eating protein food, exercising, and watching those calories. I highly recommend that you drink 4-5 liters of water every day to detox your body. A dietician will design a pulmonary exercise program for you that will give you a focus and help you.
Vaccinations
Chronic obstructive pulmonary disease is a debilitating disease and will put a considerable strain on your body, this could mean that your body is more open to getting infections, so we recommend that you go to your doctor or local pharmacy and get the winter flu vaccine and the once only pneumococcal jab.
Weather
The atmosphere can be very hot or very cold depending on where you live, these adverse weather conditions can cause you to have problems with your breathing, so if you are going outside always make sure to have a good supply of your COPD medication with you in case the weather triggers a flare up.
Be careful what you breathe
As you are probably aware, there are a few things to look out for that may cause a COPD flare-up, these include:
- Car exhaust fumes
- Dust
- Hairspray
- Car air fresheners
- Strong-smelling perfume
Serrapeptase the well-known enzyme has been used for a long time to help people with COPD. It is natural and can help with mucus buildup and lung inflammation.
Click here to read what people who have used Serrapeptase for COPD are saying.
References:
https://www.nhlbi.nih.gov/science/lung-diseases
https://www.nhs.uk/conditions/chronic-obstructive-pulmonary-disease-copd/living-with/
http://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(COPD)
Related Articles:
Search
Categories
- Adrenal fatigue
- Aging
- Beauty Products
- Beauty Products
- Bladder Health
- Blocked fallopian tubes
- Blood Flow
- Bones
- Calcification of the arteries
- Carpal Tunnel Syndrome
- Cholesterol
- Circulation
- CLE Holistic
- Copd Emphysema
- Diabetes
- Endometriosis natural treatment
- Erectile dysfunction
- Eye health
- FAQ
- Female health
- Gout
- Gut Health
- Hair loss
- Heart disease
- Heartburn
- High Blood Pressure
- Hip Bursitis
- Hip leg pain
- Ice Barrel
- Immune system
- Indigestion
- Inflammatory Diseases
- Liver Function
- Medical questions answered by a Doctor
- Memory
- Mental health
- Migraines
- Mitochondrial
- Muscle loss in old age
- Nerve Vitamins
- Numbness tingling
- Peyronies disease
- Posts
- Premature ejaculation
- Probiotics
- Prostate
- Scar Tissue
- Sexual Health
- Sinus Infection
- Sleep disorders
- Stress
- Supplements reviews
- TESTIMONIALS
- Testosterone
- Trace minerals
- Vitamins
- Weight loss supplements
Newsletter
Sign up and stay informed
Synergy Hearth & Health
Thank you!
You have successfully joined our subscriber list.